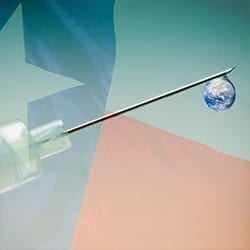
Has Texas become a conspicuous “hot zone” for dangerous tropical infectious diseases? And if so, what might that imply for the future?
In culture, history, and geography, Texas is almost a country unto itself, its population (reaching 30 million) and economy ($1.4 trillion) roughly the same as Australia. And more than almost any other part of America, it is innately and acutely vulnerable, in need of urgent action to prevent infectious diseases from becoming widespread within its borders and beyond to other parts of the United States.
In 2014, the Western Hemisphere’s first and only outbreak of Ebola virus infection occurred in Dallas, when Thomas Eric Duncan, a Liberian, traveled to Dallas to be united with his son and fiancé. Houston is today at considerable risk of a Zika outbreak this summer, which may translate into clusters of infants born with severe brain damage. That would follow Houston’s experience in 2003 — America’s first urban epidemic in decades of dengue fever, another virus infection transmitted by the Aedes aegypti mosquito. Texas is also now the epicenter of Chagas disease and leishmaniasis transmission in the United States (parasitic infections transmitted by kissing bugs and sandflies, respectively), as well as murine typhus (transmitted by fleas) and West Nile virus infection. These diseases come with a high price tag. Chagas disease alone results in an estimated $800 million in lost productivity and health care costs, much of that borne by Texans.
What makes Texas America’s “ground zero” for a new wave of tropical infectious diseases?
Arguably, the single most important (and for some the most surprising) factor is poverty. Because of its large population and a poverty rate around 16 percent (near the bottom of U.S. states), Texas ranks number one or two in terms of having the largest number of people who live below the poverty line. Poverty means low-quality housing and living amidst garbage and stagnant water, all factors that boost the exposure of Texas residents to mosquitoes and other insect vectors that transmit disease.
Second, poverty in Texas combines with unchecked urbanization. Texas is one of the fastest growing states in the nation and much of that growth is in urban areas. Crowding in poor neighborhoods, in addition to making it easier for Aedes mosquitoes to feed on humans, can also overwhelm city and county services, most importantly sanitation, access to health care and availability of affordable groceries. These additional factors increase the risk of diarrheal disease and malnutrition among the urban poor.
A third driving factor: Texas is a burgeoning global commercial and migration hub. Its coastal gateway ports of Houston and Corpus Christi will expand as an enlarged Panama Canal directs greater shipping traffic toward Texas, bolstered by expanded Asia-Panama-Texas trade. These deepening links to Asia and elsewhere will increase the region’s vulnerabilities to Asian influenza strains, as well as other pathogens such as SARS and Enterovirus 71. Houston also benefits from considerable trade, high air traffic volume and migration from West Africa: it hosts one of the largest Nigerian expat communities, rooted in the oil and energy industries.
Fourth, climate change disproportionately affects sensitive zones such as the subtropical Texas Gulf Coast. The expected warmer temperatures and more extreme alterations of flood and droughts will create additional and ideal habitats for insect vectors.
All of these globalizing forces — poverty, urbanization, climate change, commerce, and migration — have mixed to ensure that Texas will remain an epicenter of our nation’s neglected and emerging infections.
So what is to be done?
Texas does have impressive capacities. It has put in place a sophisticated system of emergency management and preparedness to handle floods, tornadoes, hurricanes, and other disasters. It boasts very good state, county, and city health departments, with outstanding and committed public health leaders and professionals. But these health departments, like most health departments across the country, lack resources.
Given their special importance for global health security, Texas health departments now require heightened investments and better tools to truly protect Americans from evolving infectious and tropical disease threats. Globalization is not going away, and additional funding from federal, state, or private sources will be essential. There is a need to enhance active surveillance activities for determining when tropical infectious diseases arise and how they are transmitted. The most obvious example will be Zika in the upcoming spring-summer-fall mosquito season in coastal Texas, but there are many other diseases to consider. There are unmet requirements for disease prevention and health education. And the time is ripe for innovation. Texas has already taken the promising step of creating the Cancer Prevention Research Institute of Texas (CIPRIT) to fund cancer research for Texas scientists; a similar program for tropical and infectious diseases research and development should be given serious consideration.
Texans in the coming decades will see continued threats from tropical and infectious diseases. The answer is not to build a wall, or rely on ad hoc, half measures, and delay action only until a crisis materializes. The answer is to elevate the priority of meeting these challenges early and preemptively — alongside other natural disasters. That requires elected political leaders acting now to finance and build capacities.
J. Stephen Morrison is the senior vice president and director of the Global Health Policy Center at the Center for Strategic and International Studies.
Peter J. Hotez is a fellow in disease and poverty at the Baker Institute and dean of the National School of Tropical Medicine at Baylor College of Medicine.